
Causes
-
Wear and Tear: Aging causes spinal discs to lose their flexibility, making them prone to damage.
-
Injury: Sudden heavy lifting or an accident can lead to a disc herniation.
-
Repetitive Movements: Activities involving frequent bending or twisting may put stress on the spine.
-
Genetics: Some people inherit a predisposition to developing herniated discs.
General Symptoms
-
Persistent back or neck pain.
-
Worsening symptoms during certain movements or prolonged sitting.
Common Causes of Lumbar Disc Herniation
Lumbar disc herniation can happen to anyone, but certain factors increase the risk:
-
Age: As you grow older, discs naturally wear down and lose flexibility, making them prone to damage.
-
Injury: Sudden trauma or heavy lifting with improper posture can cause the disc to herniate.
-
Repetitive Strain: Jobs or tasks that involve frequent bending, twisting, or heavy lifting may contribute to disc herniation.
-
Genetics: Some people inherit a tendency for weaker discs.
-
Lifestyle: Lack of exercise, smoking, or being overweight can put extra strain on your spine.
Symptoms Lumbar Disc
Herniation Can Cause a Range of Symptoms:
-
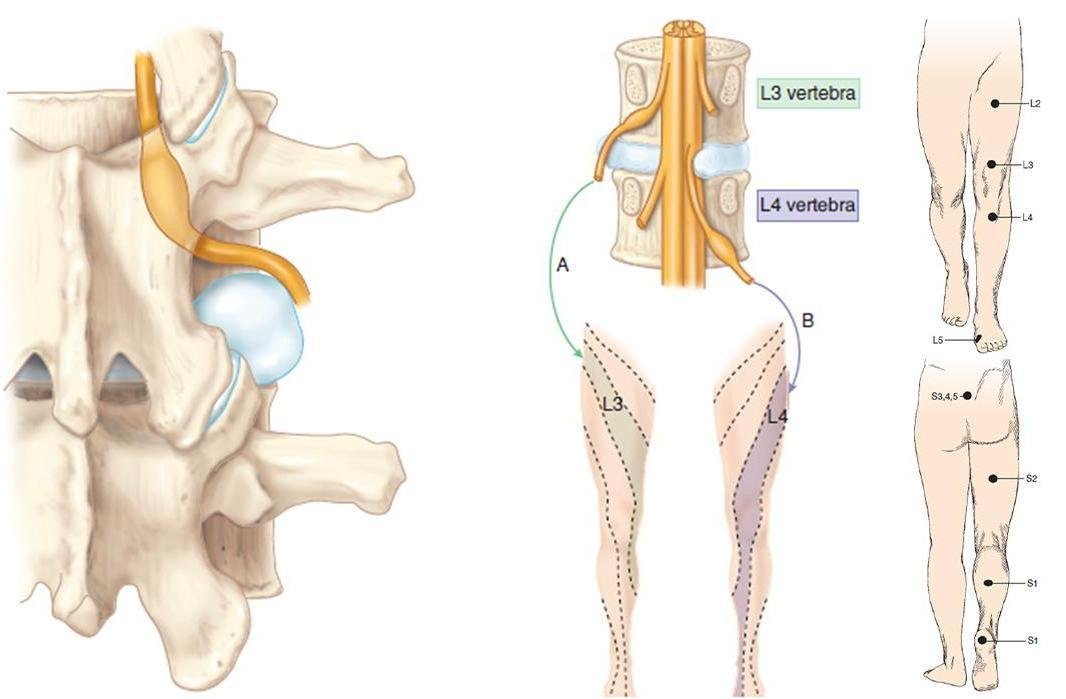
Lower Back Pain: This is the most common symptom and may feel sharp, burning, or dull.
-
Pain That Travels: Pain may radiate down the leg (sciatica), usually on one side.
-
Numbness or Tingling: These sensations may occur in the lower back, buttocks, or legs.
-
Weakness: You might feel weak in the affected leg or find it harder to lift objects or walk.
-
Bladder or Bowel Issues: In severe cases, difficulty controlling urine or stool could indicate a medical emergency called cauda equina syndrome.
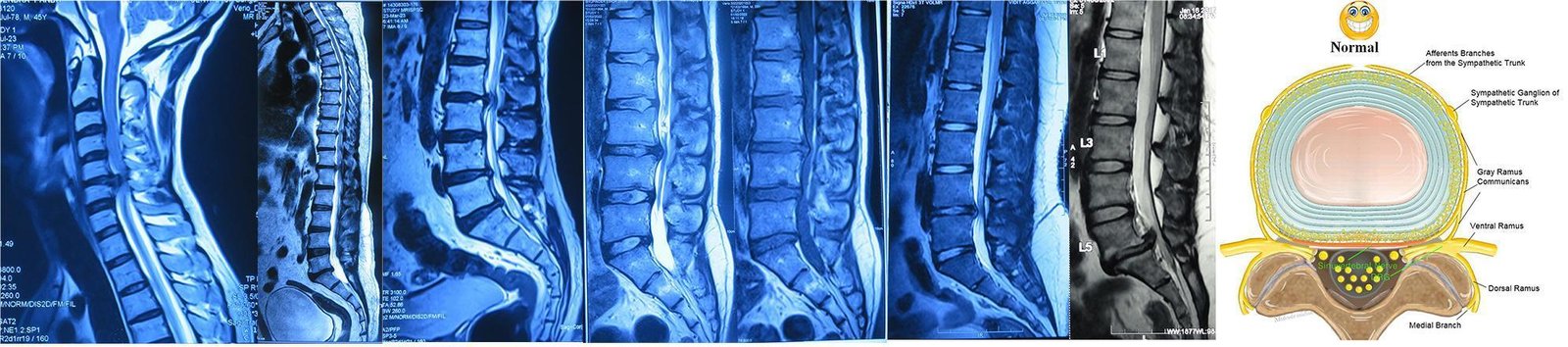
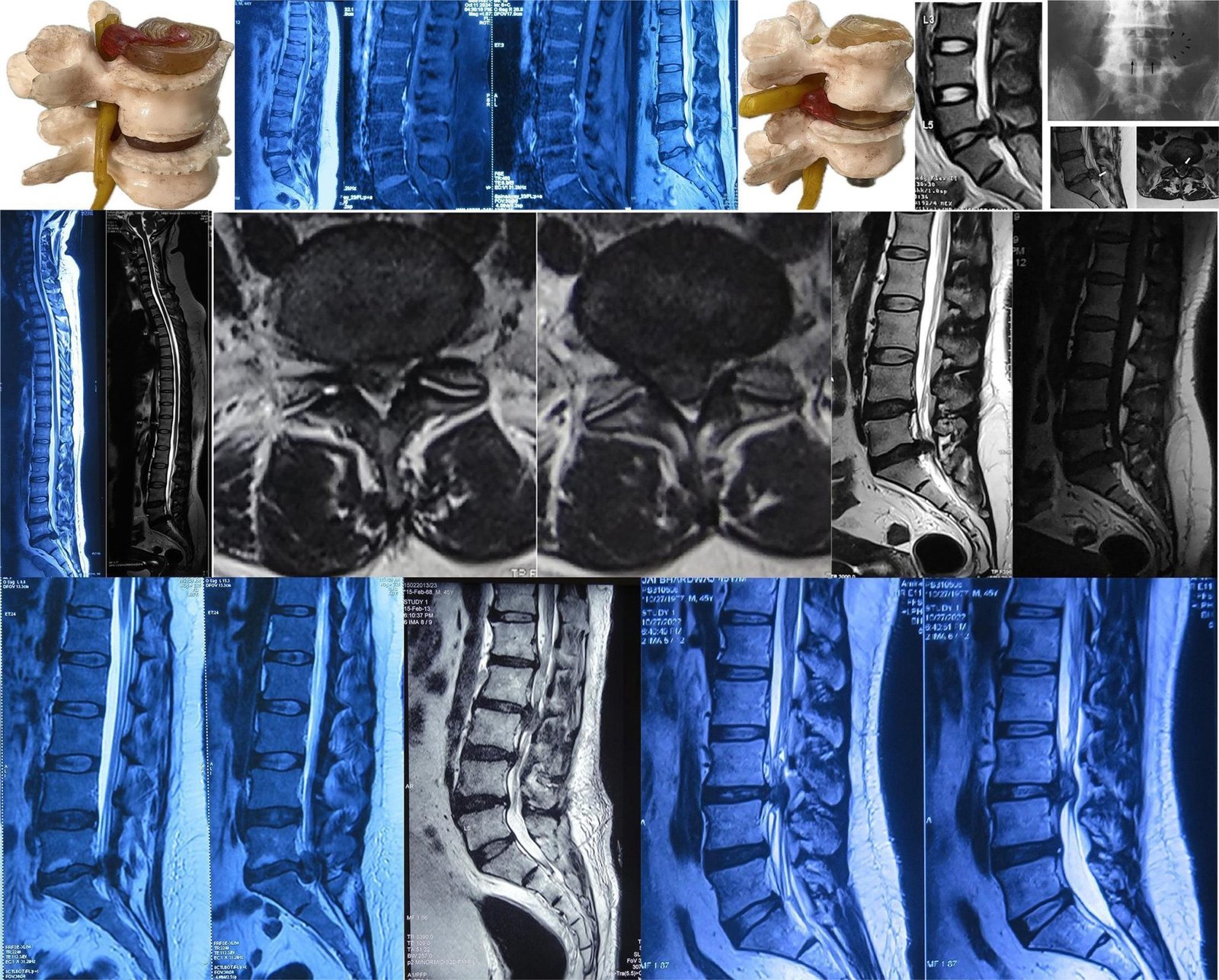
How is Lumbar Disc Herniation Diagnosed ?
To diagnose lumbar disc herniation, your doctor will:
-
Ask About Symptoms: Sharing details about your pain, numbness, and lifestyle helps guide the diagnosis.
-
Perform a Physical Exam: Your reflexes, muscle strength, and ability to walk or bend will be checked.
-
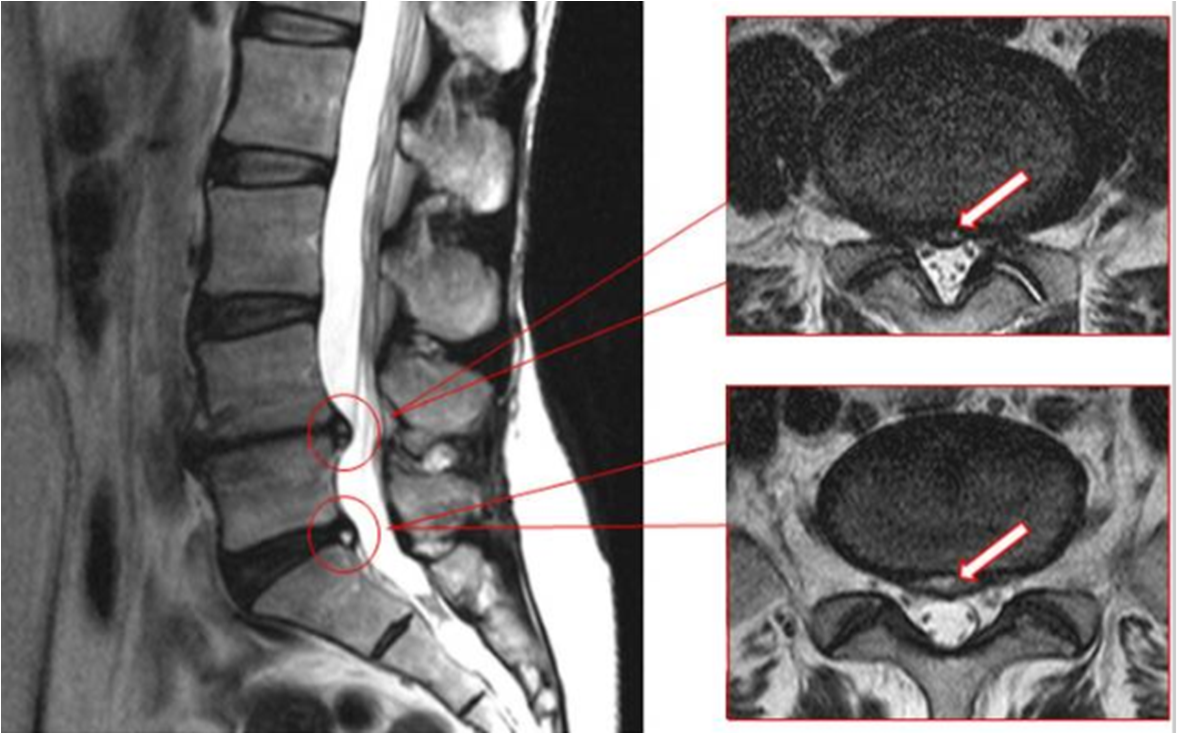
Order Imaging Tests:
-
X-rays: To rule out other causes of pain, like fractures.
-
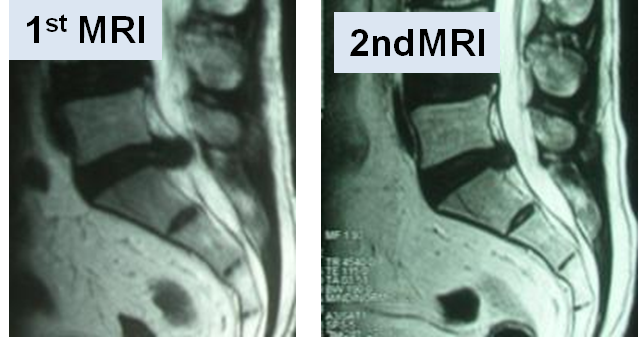
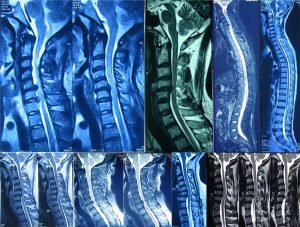
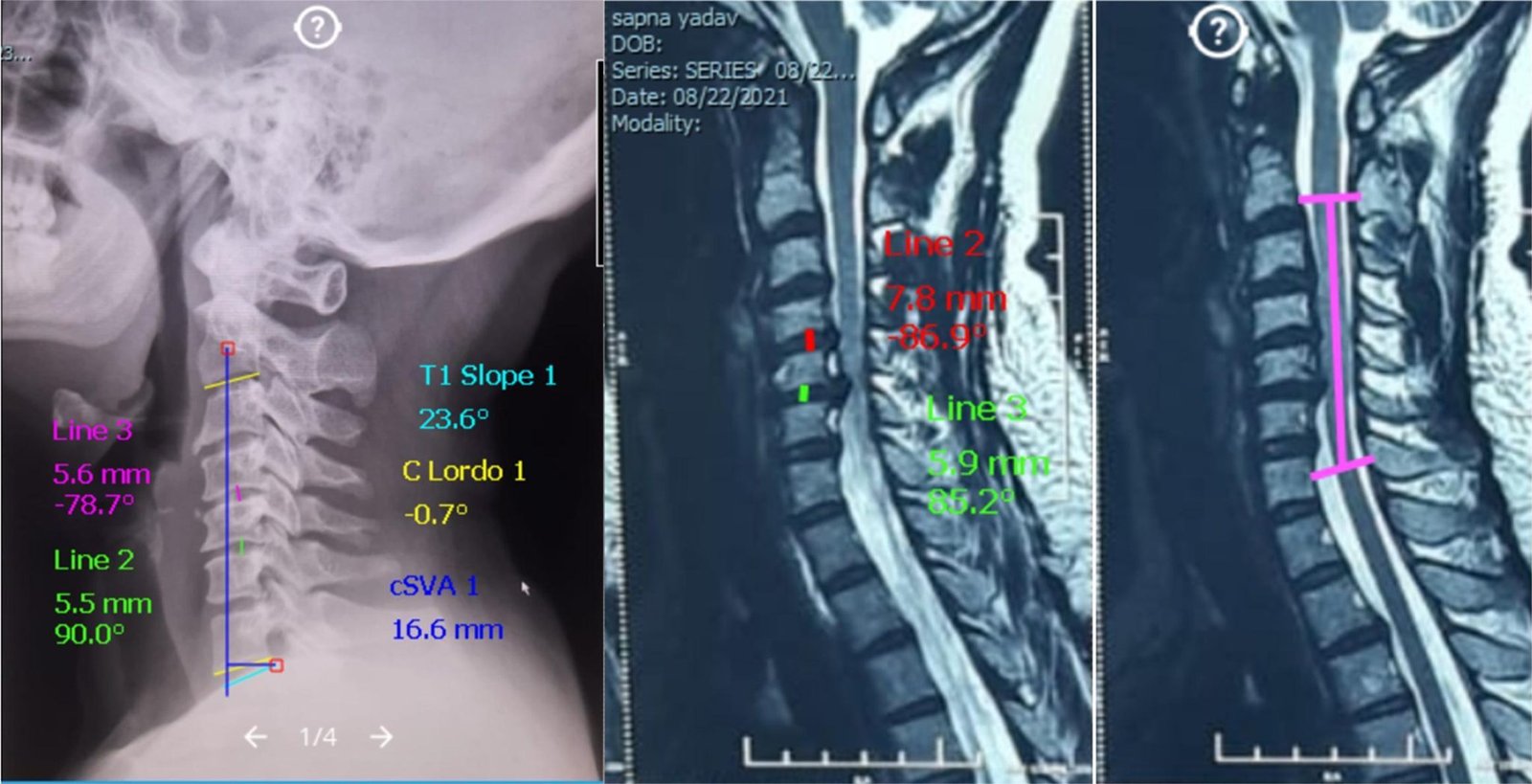
MRI: Provides a detailed view of the disc and surrounding nerves.
-
CT Scan or Myelogram: Sometimes used to confirm the diagnosis.
Treatment Options
1. Non-Surgical Treatments
-
Rest and Activity Modification: Avoiding heavy lifting or prolonged sitting can reduce strain on the spine.
-
Medications: Over-the-counter pain relievers or anti-inflammatory drugs can provide relief.
-
Physical Therapy: Strengthening and stretching exercises improve flexibility and support the spine.
-
Heat and Ice Therapy: Helps reduce pain and inflammation.
-
Epidural Steroid Injections: A shot near the affected nerve can offer temporary relief.
2. Surgical Treatments
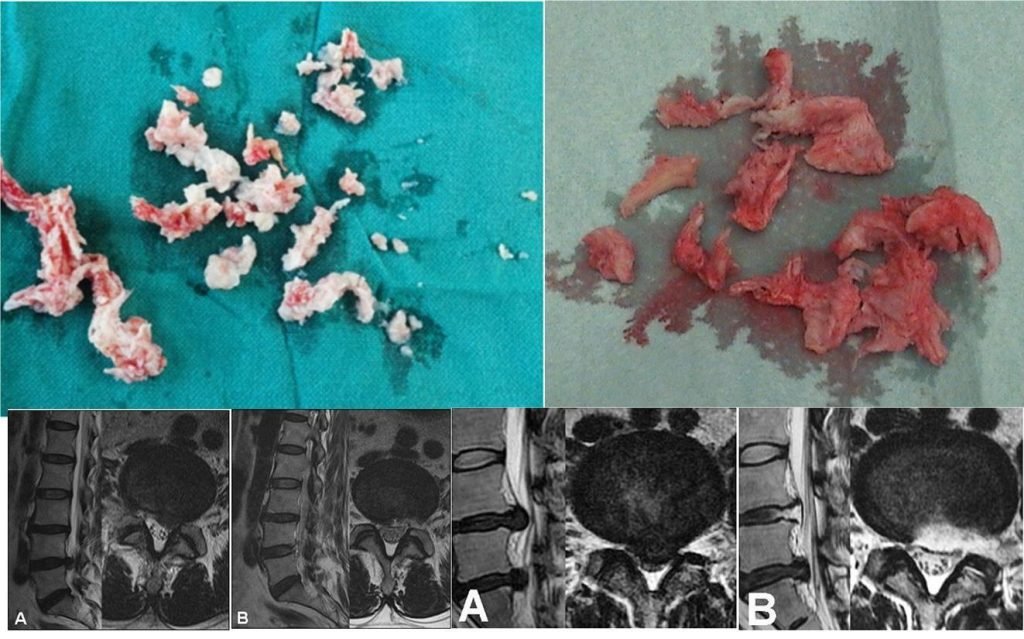
If non-surgical methods don’t work or symptoms worsen, surgery may be needed. Dr. Shankar Acharya specializes in modern, minimally invasive techniques, which ensure faster recovery and less pain.
-
Microdiscectomy: A small portion of the herniated disc is removed to relieve nerve pressure.
-
Laminectomy: In some cases, part of the bone around the spinal canal is removed for extra space.
Preventing Lumbar Disc Herniation
Simple lifestyle changes can protect your spine:
-
Exercise Regularly: Strengthen core muscles to support your back.
-
Maintain Good Posture: Sit, stand, and lift properly to avoid strain.
-
Stay Active: Avoid prolonged sitting, whether at work or home.
-
Quit Smoking: Smoking accelerates disc degeneration.
-
Healthy Weight: Extra weight adds pressure to your lower back.
Symptoms
-
Neck Pain: Often sharp or burning, it may radiate to the shoulders or arms.
-
Numbness or Tingling: A “pins and needles” feeling in the arms, hands, or fingers.
-
Weakness: Difficulty lifting objects or gripping, due to weakened muscles.
-
Headaches: Pain at the base of the skull or spreading to other areas.
Causes
Cervical disc herniation can happen for several reasons, including:
-
Age-Related Wear and Tear: Over time, the discs lose flexibility and become more prone to injury.
-
Sudden Injury or Trauma: Accidents or heavy lifting can put excessive pressure on the spine.
-
Repetitive Strain: Activities involving repetitive neck movement or poor posture can increase the risk.
How is it Diagnosed ?
If you have persistent neck pain or other symptoms, a doctor may recommend:
-
Physical Examination: Checking for pain, weakness, or numbness in the neck, arms, and hands.
-
Imaging Tests: X-rays, MRIs, or CT scans to identify the herniated disc and assess nerve compression.
-
Nerve Tests: Occasionally, tests like EMG (electromyography) to evaluate nerve function.
Treatment Options
Treatment depends on the severity of symptoms and may include:
1. Non-Surgical Methods:
-
Medications: Pain relievers, anti-inflammatory drugs, or muscle relaxants.
-
Physical Therapy: Exercises to strengthen neck muscles and improve posture.
-
Lifestyle Changes: Adjusting activities to avoid strain and improve ergonomics.
-
Cervical Collar: Temporary use to support the neck and reduce pain.
2. Minimally Invasive Procedures:
-
Epidural Steroid Injections: To reduce inflammation and relieve pain.
3. Surgical Intervention (for severe cases):
-
Discectomy: Removal of the herniated portion of the disc to relieve pressure on the nerve.
-
Spinal Fusion or Artificial Disc Replacement: Stabilizing the spine or replacing the damaged disc.

Can Cervical Disc Herniation Be Prevented?
While not all cases are preventable, you can reduce the risk by:
-
Maintaining good posture, especially during long hours of sitting or computer work.
-
Avoiding heavy lifting or repetitive neck movements without proper technique.
-
Staying physically active to strengthen the muscles supporting your spine.
-
Using ergonomic furniture and equipment.
When to See a Doctor?
-
Persistent or worsening neck pain.
-
Numbness, tingling, or weakness in the arms or hands.
-
Difficulty performing daily tasks due to reduced strength or mobility.


